Abstracts
Abstract
While the COVID-19 pandemic and recovery unfold in real time, this article investigates some of the major themes on preparations for the next pandemic. Humanity cannot rely on modern medicine to beat the coming ‘disease X’ and the world cannot afford the extortionate health and economic policy interventions during the COVID-19 pandemic again. From the COVID-19 pandemic we learned that the international economic organizations suffered from disaster myopia and that the self-image of the advanced economies is distorted. It also has become apparent that ‘beggar-thy-neighbor’ health care was generally practiced while global health care should have been the norm. A discussion on the related issues of rationing, triage and scarcity of health care during a pandemic is urgently needed. All in all, a major global investment project is necessary to reduce the vulnerability to and impact of pandemics. As inequalities to a large extent determine pandemic vulnerability, an adjustment of Sustainable Development Goals (SDG) is necessary.
Keywords:
- covid-19,
- pandemic preparedness,
- global public goods,
- long-term strategy
Article body
1 Introduction
Vaccines have not been the gamechanger people hoped for. It is both important and encouraging that vaccines against the coronavirus have been developed at warp speed in widely differing political and economic systems and that the world vaccination rate two years after the outbreak of COVID-19 surpassed the sixty per cent level. These are unprecedented achievements, but unfortunately not enough. Many countries in the Global North have significant subcultures that distrust authorities and for religious or other reasons do not want to be vaccinated. At the same time, many people in the Global South that would like to be vaccinated still have not had the opportunity to get a vaccine. Therefore, significant breeding grounds for new variants continue to exist, both in advanced and developing countries. The emergence of the omicron variant is a strong reminder that the vaccination record is no reason for complacency but rather an additional reason to think about the future with an endemic COVID-19, a period that paradoxically will be both post-pandemic and pre-pandemic.
This is the more so, because COVID-19 is certainly not the last pandemic that humanity will experience. The frequency of pandemics actually has increased since 1700 despite enormous improvements in medical technology, housing, hygiene and living standards (Figure 1). The reason is that health care improvements and social development were outpaced by higher pandemic risk. This risk is associated with global travel, human–wildlife interaction, intensification of global food production, and densification of population (Daszak, 2012).
Indeed, in 2020, the emergence of a contagious virus should not have come as a surprise, yet ‘preparedness’ to deal with such an emergency was below standards (Sathyamala, 2021). A very serious policy error has been the lack of preparation of the population and the business sector for lockdowns. The issue is that none of the pandemic protocols in the advanced economies in 2019 prescribed the massive use of so-called Non-Pharmaceutical Interventions (NPIs) for a pandemic that did not meet the threshold of the Spanish Flu – which COVID-19 did not by any standard.[1]
Figure 1
Number of pandemics per decade
A similar point can be made regarding economic policy preparation. A myth exists that the COVID-19 pandemic and its impact could not have been foreseen in 2019. According to the IMF’s Economic Counsellor,
[a] pandemic scenario had been raised as a possibility in previous economic policy discussions, but none of us had a meaningful sense of what it would look like on the ground and what it would mean for the economy
Gopinath, 2020, p. v
Likewise, in an overview article, Rasul (2020, p. 265) characterized the literature on viral outbreaks as a ‘nascent literature’. Economic analysis of epidemics and pandemics and their impact was, however, not embryonic at the end of 2019. Before COVID-19, leading economists already stressed the risks and dismal consequences of ‘disease X’: ‘Few doubt that major epidemics and pandemics will strike again, and few would argue that the world is adequately prepared’ (Fan, Jamison and Summers 2018, p. 129).[2] Also, policy makers at the World Bank were well-aware of the devastations of Ebola and HIV/AIDS on the ground (World Bank 2014). There are quite a few indications that other international organizations basically ignored the topic. Sands et al. (2016), for example, point out a lack of analyses of the economic impact of pandemics by global and regional institutions. They provide a detailed analysis of economic reports regarding fifteen countries that were most severely hit by SARS, MERS, Ebola and Zika. Focusing on the two years before these outbreaks, their findings show complete ignorance of epidemic risk in the IMF Article IV consultations. Consequently, institutional preparation for a pandemic was low (International Working Group on Financing Preparedness, 2017).[3]
It is no exaggeration that the pre-COVID-19 self-evaluations of the advanced economies in Europe and the United States show that they suffered from disaster myopia and cognitive dissonance. To specify, international organizations had pointed out that the lack of preparedness was mainly a problem of the non-OECD countries. A fairly random example is the 2017 World Bank study Disease Control Priorities: Improving Health and Reducing Poverty, that reports:
A geographic analysis of preparedness shows that some areas of high spark risk also are the least prepared. Geographic areas with high spark risk from domesticated animals (including China, North America, and Western Europe) have relatively higher levels of preparedness although China lags behind its counterparts. However, geographic areas with high spark risk from wildlife species (including Central and West Africa) have some of the lowest preparedness scores globally, indicating a potentially dangerous overlap of spark risk and spread risk.
Madhav et al., 2017, pp. 320 – 321
Even though the fallacy and peril of this perception were acknowledged, no action was undertaken (Commission on a Global Health Risk Framework for the Future 2016, International Working Group on Financing Preparedness, 2017, World Health Organization 2019). The inconvenient truth is that the world has been busy fighting COVID-19 since early 2020, but that no real steps have been set to significantly increase pandemic preparedness: the post-COVID-19 world is simply as ill-prepared as the pre-COVID-19 world. One of the most disturbing facts has been the lack of a truly global approach to the pandemic. To a large extent, this gap does not come as a surprise: health care policies by and large have remained in the national and state realm even if sovereignty in other government activity areas was transferred to higher federal or supranational levels (Saltman 2008). The reason is that health care is of direct impact for the franchise: voters care about their health a lot and therefore national and local politicians want to be in charge. What came as a surprise, however, is that competition between states/provinces for medical emergency supplies was fierce. For instance, in the US, the competition was not only observed between the individual states, but also between the federal government and the states (Polifact, 2020). The inconvenient truth is that health care during a pandemic is one of the few remaining fields where raw and unrestricted beggar-thy-neighbor policies flare up.
Many valuable lessons have been learned thanks to COVID-19, some positive and some negative. On the positive side are the blossoming digital economy and its ease of working and connecting while sheltering at home. On the negative side we have learned the costs of lockdowns and the toll of the prioritization of COVID-19 over existing diseases. Since these societal costs are an increasing burden, future NPIs need to be designed more intelligently, helping countries to restructure and support the transition from a basically ignorant and domestically oriented society into a global pandemic-aware civilization.
So far pandemic policies have been by and large national, mono-viral, monodisciplinary and focused on the short term. This article aims at broadening that focus and time horizon. Section 2 argues that we can not necessarily rely on modern medicine to beat the next ‘disease X’, and that a major global investment project is required to reduce vulnerability to and impact of pandemics. Section 3 develops a political economy perspective on pandemics. Section 4 focuses on inequalities that to a large extent, determine pandemic vulnerability and discusses the relationship with SDGs and development cooperation. Section 5 addresses the related issues of rationing, triage, and scarcity of health care during a pandemic. This is a politically painful and morally difficult topic to confront, but a challenge that economists cannot avoid. Section 6 offers some concluding thoughts.
2 Modern medicine is not a panacea for the next pandemic
We cannot simply rely with confidence on a medical cure for the next pandemic despite humanity’s success in developing vaccines against COVID-19. Firstly, many of the medical interventions, new drugs and vaccines are not nearly as effective in the real world as commonly thought, because significant parts of the population prefer to rely on their immune system and neither want to use (insufficiently tested) drugs with potential long-term impacts, nor to adhere to social distancing and related NPIs. What we have learned is that behavior, trust and perceptions matter a lot (Seyd and Feifei 2021; Marugg and Schweinberger, 2021). Anti-vaxxing is widespread in many countries and neither NPIs nor vaccination (and vaccine passports) can solve the major problem of a pandemic – that is: the increasing risk of a breakdown of the health care sector (Gans 2021; Dasaratha 2021).
Second, the next pandemic could be a completely new ‘disease X’ for which no apparent medical solution is available. Comparing modern pandemic preparedness with the situation during the Spanish Flu in the 1910s, Morens and Fauci (2007, p. 1025) concluded a decade ago that ‘Almost all “then-versus-now” comparisons are encouraging, in theory’. Their ‘in theory’, however, is not an innocent academic caveat: antiviral and antibiotic resistance, medical capacity constraints and the vulnerability of the just-in-time character of the medical supply chain are by now familiar problems. Indeed, we may not even be able to find a vaccine against the next virus attack (Lassa Fever is an example of such a disease with pandemic potential; see Salami et al., 2020). The omicron variant has demonstrated that a mutating virus can and will avoid vaccine defenses.
Third, we know that the key medical inputs (i.e., well-trained staff and access to high quality facilities) cannot be stock piled. During a pandemic these inputs will always be in short supply and due to the exponential character of an outbreak, higher levels of medical machines and personal can only buy very limited time.
Fourth, COVID-19 has revealed the ‘paradox of medical and social achievement’: the impressive worldwide life expectancy increase has amplified pandemic vulnerability. Figure 2 illustrates this paradox. Countries with comparatively young populations are associated with lower COVID-19 deaths per million population. Countries with comparatively older populations could achieve relatively low death rates, for example, if they follow an elimination strategy with very strict lock downs and border procedures, but typically the impact of uncontrolled outbreaks are higher for these countries.
Figure 3 further delves into this paradox by providing a counterfactual for the Spanish Flu and COVID-19 based on mortality rates by age cohort (historic data and forecasts for the world population).[4] In the 1950s, COVID-19 would have hit a younger world population, and like the 1957–1958 Asian flu pandemic, it would have been serious, but from a longer time perspective, relatively mild as the comparison with the Spanish Flu counterfactual shows. By 2070, however, the world’s population – thanks to further medical and economic progress – will have aged so much that the same coronavirus (‘COVID-69’) would ‘beat’ the Spanish Flu.
Figure 2
Covid deaths and median age
Note: for readability of the graph Peru has been excluded.
Figure 3
Hypothetical death rate of Spanish Flu and COVID-19
These paradoxes have wider implications. Over the past decades, medical performance has been so good that the world did not prepare for a medical breakdown, especially in many advanced economies. Here, both the general public and policy makers had difficulty imagining a life-threatening situation that modern medicine could not handle. These paradoxes probably drove the policy response to the pandemic, that ultimately was the true Black Swan of the pandemic: for the first time in history, closing entire economies was used as a medical tool applied at more or less the same time and worldwide.
Figure 4
Cumulative stringency and COVID-deaths per million population* (G20 countries and world average indicated)
Note * In order to improve readability the figure excludes Peru, Bulgaria, Bosnia and Herzegovina, Hungary, Czechia and Georgia which all had a death rate exceeding 3000 per million inhabitants
This brings us to the fifth reason why we cannot exclusively rely on medical solutions for the next pandemic: a pandemic is not so much a purely medical problem, but rather an epidemiological-economic crisis (Shami and Lazebnik, 2021). COVID-19 laid bare the limits to the use of NPIs. In many western democratic market economies public health measures have been imposed lukewarmly, seeking, so to say, a balance in the pandemic trilemma that trades-off healthcare, freedom and the economy (Diagram 1).
Diagram 1
The pandemic trilemma
Note: The trilemma is that countries cannot achieve full respect of individual liberties, complete economic freedom and universal access to health care at the same time during a pandemic. It is possible to choose two out of three but impossible to have all three at the same time.
Figure 4 presents data on cumulative stringency, that is: the summation of the daily scores of the Oxford COVID-19 Government Response Tracker (Hale et al. 2021) since the start of the pandemic. Cumulative stringency offers an indication of the quantity of restrictions over the pandemic. This snapshot makes four points. First, China (at the bottom right) stands out as one of the countries with the most stringent measures and a low death rate. Second, the worst performing G7 countries over time have taken almost as much liberty away from their population as China did in comparatively short bursts of extremely high stringency, but they have a much higher death rate. Third, the outcomes on the European continent vary widely suggesting that country specific characteristics (including culture, institutions and policies) matter. Fourth, a comparison between Asia and Europe likewise underscores the importance of the organization of society (see also Wyplosz, 2020 and Farzanegan, 2021).[5] NPIs appear to be less fit for Western democracies that value the individual more than the collective.
Because of the obvious limits to medical solutions, we need to prepare and find ways to structurally mitigate the impact of a contagious disease on the move. Humanity needs to work hard on ‘pandemic management’ just as disaster management has been developed. Our main efforts need to develop more intelligent ‘non-pharmaceutical interventions’ – more intelligent than the short-term measures that we have used in 2020 and 2021.
3 A political economy perspective
COVID-19 is not the worst medical problem of our generation (AIDS, for example, caused 26-46 million deaths and yearly HIV infections are still to the tune of 1-2 million) and neither is the current recession the worst economic disaster since the Second World War. The narrative that the COVID-19 pandemic created the worst disaster of our lifetime has been voiced by a great many economists. Equally common is the idea that our current economic woes are an economic disaster that only has found its equal in wars and the great depression. Clearly the observation for the year 2020 that more than 95% of the world’s countries/areas experienced negative economic growth is without historic precedent, but Figure 5 reveals that for many individual countries the size of the economic impact of COVID-19 is less exceptional that often argued
The bars in Figure 5 report the number of years in the period 1901-2019 that had a contraction in excess of the covid crunch in the year 2020. The grey bars report the number of years during wartime (black bars are peace time contractions). The dots for ease of reference provide the growth rate in 2020. Only for Panama, Ecuador, and Colombia the Covid contraction has been the largest on record since 1901. Figure 5 therefore illustrates that large economic contractions are much more frequent than often assumed in analyses of the COVID-19 crash. By implication economic resilience after severe external shocks is much larger than often acknowledged.
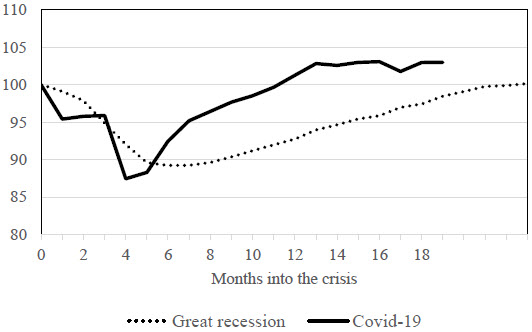
Figure 6 puts the issue of resilience during the pandemic further into context, shifting the focus from individual country experiences to the global level. The graph reports data for world merchandise trade (top panel) and world industrial production (bottom panel), comparing the Great Recession and the COVID-19 collapse. The key data source for the assessment is the CPB World Trade Monitor, which aggregates worldwide monthly data on merchandise trade and industrial production for a sample of 81 countries that together account for 99% of world trade (Ebregt 2020). The black line represents the COVID-19 data; the dotted line shows the experience during the Great Recession.
Figure 5
Number of years where per capita GDP decreased more during 1901-2019 than in 2020
Both crises are characterized by significant drops in economic activity in the first half year, but recovery during the pandemic is much faster, both for world merchandise trade and for world industrial production, than during the Great Recession.[6] Similar resistance can be observed with respect to capital flows such as remittances and Official Development Assistance (World Bank 2021) and to a somewhat lesser extent for Foreign Direct Investment (UNCTAD 2021).
Figure 6
World trade and world industrial production during the Great Recession and the COVID-19 collapse (index numbers; start of crisis=100)
Figure 6a
World merchandise trade
Figure 6b
World industrial production
In view of this apparent resilience of the world economy, the problem thus is not so much whether the world can survive a pandemic outbreak; the issue is rather if recovery is quickly enough so that the challenges of the next pandemic can be met with confidence. A pandemic is a ruin problem: a high impact event with a high probability of surviving a single event but a low probability of surviving repeated exposures (Norman, Bar-Yam, Taleb 2020).
A clear example of the ruin character of pandemics can be found in public finance (see also Alm et al. 2021 and Shami and Lazebnik 2021). Figure 7 takes a long-term perspective and starts after the Second World War. Reliable estimates for Gross Planetary Product are not available for that point of time and therefore the graph starts by showing the debt level for the G7 countries until around 1980. In the 1950s, 1960s and early 1970s the debt-to-GDP ratio decreases thanks especially to the strong growth record of the Golden Age of Capitalism, but the Oil Crisis of 1973 and the ensuing period of stagflation forced a turning point on that trend. The upward trend is illustrated for the advanced economies and – starting in the year 2000 – is confirmed at the world level. The outbreak of the Corona crisis is associated with a large increase in the debt-to-GDP ratio both via the nominator (higher deficits) and the denominator (slower growth). The recovery of economic growth in 2021 does not bite into the debt to GDP ratio.
Figure 7
Gross government debt in percent of regional GDP (1950–2021)
For the advanced economies, Figure 7 clarifies that this country group experiences indebtedness in excess of the high debt-to-GDP ratio reached at the start of the 1950s because of the war efforts and the massive destruction during the Second World War. This is a worrisome level, also because current projections do not foresee a return to pre-COVID-19 levels. Clearly then the room for maneuver (that from a historic perspective was limited to start with) has reduced further due to ‘pandonomics’. One of the unavoidable consequences is that we need to increase the policy space again. Debt-to-GDP ratios need to be steered down to reasonable and sustainable limits. If not, an economic policy response to the next pandemic will be impossible.
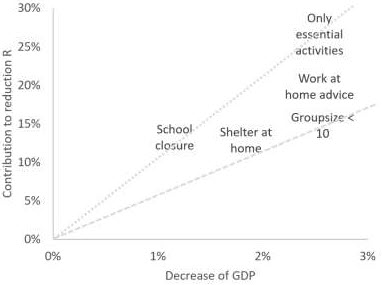
In the short term the cost efficiency of NPIs needs more attention. The spread of the NPIs and the economic support measures to address the economic fallout of the NPIs is remarkable. Baldwin and Weber di Mauro (2020a,b) already foresaw that COVID-19 would be as contagious economically as it is medically. This ‘natural policy experiment’ shook the world with a multifaceted cluster of health policies as well as fiscal and monetary policies. The heterogeneity of the impact of the pandemic on life and livelihoods as well as the diversity of strategies and policies provide a unique data rich environment that will allow detailed answers on what measures work and what policies are better to avoid.[7] From a purely medical perspective the impact of NPIs on infections is the key target. From a purely economic point of view the impact of NPIs on the economy is key. From a sensible policy perspective considered measures need to be evaluated on the basis of both medical impact and economic impact. Which lockdown measures offer the best balance between the benefits (decrease of virus transmission) and the costs (GDP contraction)?
Figure 8 provides some insight into this for a number of lockdown measures, based on a recent regression analysis for the OECD countries and the pandemic period up to and including May 2021. School closure appears to be the most cost-effective (the ratio between benefits and costs is shown by the dotted line), limiting the group size to less than ten persons (dashed line) the least; this is also the most expensive measure. These findings are supported for other infectious diseases and methods. (Adda, 2016; Inglesby 2006). Of the five measures studied, the closure of all economic activities (with the exception of the essential sectors) results in the strongest reduction in the reproduction number R.[8] The economic costs are obviously correspondingly high, but the measure is more cost-efficient than other measures that reduce R to a lesser extent and at higher marginal costs.
Figure 8
Reduction of reproduction number R and GDP growth due to NPIs in the OECD
In the same vein, an evaluation would seem to be possible regarding an elimination strategy versus a mitigation/suppression strategy or for short (presumably stricter) lockdowns versus protracted (presumably more relaxed) lockdowns. As to the former, König and Winkler (2021) find for a panel of 44 countries in 2020 that an elimination strategy comparatively speaking does not hurt the economy more than a suppression strategy while the health outcomes are better (a similar pattern is suggested by Figure 4 above), suggesting that the elimination strategy is more cost effective. As to the latter, cost benefit analyses typically find that short term lockdowns can have a net benefit but that longer lockdowns would imply unrealistic valuations of life (Rowthorn and Maciejowski, 2020; Allen 2021), basically because a life can only be saved once while the costs of lockdown continue. The contribution of societal cost-benefit analyses is clear. Resources are limited, and forward-looking analysis is, therefore, vital for decision making. One of the important COVID-19 lessons is that the costs of the short-term measures are becoming increasingly aggravated by unacceptable rationing of non-COVID-19 care. Moreover, the societal limits to lockdowns that require perseverance and discipline are also becoming increasingly clear, especially in Western democratic market economies. Lockdowns have worked during the first wave of the COVID-19 pandemic, but to maintain such a regime for more than a few months appears to be increasingly doubtful, if at all possible. Likewise, frequent re-vaccination strategies do not appear to be sustainable. Therefore, a long run strategy aimed at increasing societal resilience is necessary.
4 Elements of a long-term strategy for pandemics
Mitigation and adaption need to be top priorities. The trade-offs between COVID and non-COVID suffering along many dimensions are an important topic for economists because a pandemic is, in the end, all about scarcity. Significant investments will be necessary to enhance resilience. City-planning, public transportation, workplace design, social safety nets, and education will need to be rethought. An intelligent strategy should enable a major transformation, and – as an important side benefit – the public and private investments could offer an alternative to monetary expansion and fiscal indulgence that could help the economic patient recover and prepare for the next pandemic.
Preparation for the next pandemic needs to take place at five relevant levels: individual (households and firms), local, national, international, and global. It is important to realize that the strength of the defense against the next pandemic will be determined by the weakest link, and it cannot be stressed enough that all five levels of defense need to be active. Basic hygiene, masks, social distancing, and awareness provide the first line of defense at the individual level, but pandemics also require rethinking of city design and the proper roles of nations, as well as regional and global cooperation. Global pandemic management will simply not be effective if individuals are not prepared. Admittedly, individuals and firms can prepare for the next pandemic, but without global collective action their preparations will be less effective. International policy coordination and external and cross-border effects are key issues. The nation state is not always the optimal health care area and certainly not during pandemics. The EU provides a clear example of highly integrated markets with free movement of people, but national health policies in Europe that remain unsynchronized and induce flows of people to those locations where lockdown measures are less strict.
One of the basic economics lessons is that we need global public goods for a well-functioning world economy (van Bergeijk 2014). The best way forward is not so much to expand the WHO mandate but rather to use existing economic policy structures to manage the economics of delivery of these global public goods (e.g., country surveillance by IMF, OECD, World Bank, peer-review and best practices exchange). The lesson highlighting that strengthening global governance is an elementary step in pro-active pandemic preparedness, is certainly not new – it has been already drawn with respect to Ebola, AIDS/HIV, and SARS. However, our response to COVID-19 has shown again that we do need to take that lesson serious.
Perhaps the most important lesson from the COVID-19 pandemic is that inequalities are the Achilles heel of the society that is being hit by an epidemic. This is true for the full range of societal organization: the spread of disease can be delayed but in our highly globalized world cannot be stopped. We thus need to prepare for the next pandemic. The advent of a new ‘disease X’ is a certainty; only its timing is uncertain. The fact that COVID-19 is a pandemic amplifies our current problems, but even for new contagious diseases that do not reach all continents, inequalities are the breeding ground for disease spreading and consequent suffering. Reducing epidemic vulnerabilities requires to reduce these inequalities. But fighting the next pandemic implies that we should not limit our attention to inequalities at home, because the inequalities around the world – within and between countries – provide the hot spots and the disease pools from which new variants, viruses, and other contagious diseases emerge. The implication is that reducing inequalities in other countries and continents becomes a business proposition: an investment project with a high rate of return.
Clean water and handwashing facilities in developing countries are an example of a cheap, significant and necessary precaution for the advanced economies. SDG 6 ‘Ensure access to clean water and sanitation for all’ is an excellent business proposal that reduces pandemic vulnerability. Investing in clean water and sanitation is a very cost-effective tool to alleviate global pandemic vulnerability. Moreover, understanding that poverty is a breeding ground for pandemics implies that income inequality between and within countries is much more important than the Sustainable Development Goals (SDGs) seem to acknowledge (van Bergeijk and van der Hoeven, 2017)).
The scale of preparations cannot be international (i.e., involving many countries) but needs to be global (i.e., involving all countries). This had, of course, to some extent already been recognized before the Corona crisis by the move from ‘international health’ to ‘global health’. Pandemics, however, have not yet received the explicit attention they need in the SDGs. The SDGs (and in particular, the SDG 3 ‘Ensure healthy lives and promote wellbeing for all at all ages’) do not mention prevention of pandemics per se. Health target 3.3 ‘By 2030, end the epidemics of AIDS, tuberculosis, malaria and neglected tropical diseases and combat hepatitis, water-borne diseases and other communicable diseases’ could be easily adjusted. Target 3.d ‘Strengthen the capacity of all countries, in particular developing countries, for early warning, risk reduction and management of national and global health risks’ looks satisfactory at first sight, but it misses the point that the ‘in particular’ is equally relevant for the advanced countries. In other words, the SDGs are targets for every country independent of its level of development. This might be the most important lesson for the Global North: the advanced economies are not invulnerable, and they were ill-prepared. The Global North needs to take inequalities seriously in order to survive. Fighting inequalities globally and domestically is one of the best business propositions that we have for the Global North. It is also a highly profitable proposition.
Pandemic preparedness must cover prevention, detention, delay and mitigation. A major global investment project is necessary to enhance humanity’s resilience, and economic analysis of the societal costs and benefits is key to its success. The costs of COVID-19 and the associated health care and economic policies have been enormous. Economic damage alone (so without considering the costs of sickness and loss of life) can be gleaned from the difference between the ex ante predictions of global economic growth for the year 2020 and the ex post realization in the flagship publications of the international financial and economic institutions. Comparing the ex ante forecast for 2020 made at the end of 2019 and the actual numbers ex post for 2020 that are now being reported, the drop in global production has been to the tune of 5.9% (OECD) to 6,6% (IMF) of Gross Planet Product (about the combined size of the economies of Germany and France) and a recent, yet unofficial, estimate (Agarwal and Gopinath 2021) suggests an even 50% higher burden. Even without the consideration of human suffering (estimated at 40 trillion per century, see Jamison et al. 2018), a conservative estimate of the welfare reduction of pandemics, which are diseases of inequality, in a century would amount to €100 trillion. To put this number further into perspective, it is useful to note that UNCTAD (2014) calculated that achieving all the SDGs by 2030 will require an annual investment of 2.5% of world production (to which the private sector is expected to contribute 1.8%, leaving a financing gap of 0. 7%). Given the cost of COVID-19, increasing development assistance from the current actual 0.3% to the target of 0.7% of the national income of rich countries is both a first step and an attractive investment. And we do not need to rely on traditional modes of financing; liquidity is not an issue (Committee for Development Policy, 2020; Van der Hoeven and Vos, 2022). The contribution of achieving the SDGs to reducing the frequency and impact of pandemics is clear and these benefits exceed the costs by far. Economics alone cannot solve the pandemic problem, of course. We really need to marry medicine and economics. That requires, perhaps, the biggest investment: a mental investment to understand in a truly multidisciplinary way that pandemics are essentially about behavior and choices that need to be made on a rational basis despite the emotions related to the outbreak of a new disease.
5 Wicked problems: rationing, triage and scarcity
Policy making during a pandemic has been described as a wicked problem, not only because of the incomplete, contradictory, and constantly changing and difficult to recognize requirements but also because of the ethical and political trade-offs (Miller and Parent, 2012). Ultimately pandemics are all about scarcity. The problem is that everybody gets ill at the same time and needs access to health care. This makes health care workers and facilities extra vulnerable, and it threatens a breakdown of the health care system that would further reduce health care provision and increase scarcity. Universal health care access is impossible during pandemics as we learned from the comparatively mild case of COVID-19 when access for non-COVID related diseases was scaled down in many countries to unprecedented levels. Access at times became severely impossible for non-COVID patients and the health consequences of this restriction will only become clear in the longer term. It may be necessary to rethink health care access and prepare dedicated medical facilities for the next ‘disease X’. It may also be necessary to increase the pool of medical staff by means of conscription and mobilization.
The reasons to think outside the box are clear since the usual economic recipe in a (neo)liberal economy is irrelevant: we cannot leave this to the market because supply and demand are almost perfectly price inelastic in this situation. This means that the world is in a second-best scenario and needs to consider that rationing rather than universal access to health care is optimal during a pandemic. In this scenario many of the key economic insights are still very relevant: the economics of lockdowns is not a rocket science, and the tools to analyze short-term and long-term impacts of pandemics are available. Sophisticated analyses exist of repressed inflation and central planning (Davis and Charemza 2012) as well as rationing in a blend of computable equilibrium models, neo-Keynesian models and models for economies with non-market clearing prices. From such analyses, we can understand what happened on the markets for ventilators, medical masks and vaccines. It also showcases that ‘the phenomenon of manipulation through demand and supply leads then to a perverse phenomenon of overbidding, and to the non-existence of an equilibrium unless additional constraints are put on demands and supplies’ (Bénassy 2016). The upshot is that rationing needs to be designed and monitored properly in order to be efficient – the most important requirement is that rationing cannot be manipulated by offering or asking quantities above what is necessary. But rationing has more aspects than the market for health care equipment and also needs to consider where to restrict activity and to what extent and how access to treatment needs to be organized. Examples are Boettke and Powell (2021) who point out the welfare-theoretic suboptimality of measures that restrict activities of the young for a health care externality (of COVID-19) that emerges from the elderly or Akbarpour et al. (2021) who consider how scarce vaccines need to be rationed in a heterogeneous population.
The big issue is not in the economic technicalities but in the perceived (im)morality of rationing. Rules to allocate access to health care need to be designed since triage is unavoidable. (Triage is a form of medical rationing that determines access to health care based on the probability for survival after treatment; it is a common practice during disasters and mass accidents.). The claim that every person has the right to being treated at an intensive care facility makes no sense during disasters, and it does not make sense during pandemics either. The debate on triage and the design of efficient rationing schedules cannot be avoided. The next pandemic is coming.
6 Conclusion
One learns a lot about humanity during a pandemic. Pandemics reveal imbalances, contradictions, and inequalities that we can no longer ignore at the peril of succumbing under the pressure of the next pandemic.
We have learned that access to basic health care is not guaranteed any more during a pandemic and that marginalized groups are the most vulnerable. We have learned that essential workers are at high risk of getting infected and that society cannot survive without the people that continue to provide those essential services. We have learned that working conditions and the organization of workplaces to a large extent determine the speed of transmission of a virus and that especially low-income earners appear to work in places where outbreaks occur frequently. We have learned that marginalized poor and informal sector workers have no access to hygienic facilities and that lockdowns are not a realistic tool since their very livelihoods are threatened. We have learned that the most vulnerable clusters in society consist of people that have no opportunity to work from home, need to travel by public transportation, have low incomes, and that their housing does not allow much scope for social distancing. We have learned that this is true both for the Global South and the Global North. We have learned… I sincerely hope that we learn.
Appendices
Notes
-
[1]
See, for a detailed discussion, van Bergeijk 2021, Chapter 2.
-
[2]
Indeed, a substantial pre-COVID-19 literature exists providing detailed analyses and estimates of potential tolls of pandemics (see van Bergeijk 2021, Chapter 2).
-
[3]
Relatedly, economic policy making during a pandemic was seen as just another form of stabilization and crisis management with already well developed policy instruments (Behsudi, 2020).
-
[4]
Figure 3 is not a prediction of the final outcome of COVID-19 but simply applies estimates of mortality as approximated in the first phase of the pandemic to the world population at large.
-
[5]
A deeper investigation of different societal settings – from a Darwinian Society via a Big Brother Society to an Autarkic Autocracy – shows that bad institutions and behaviour can make us extra vulnerable, but also it illustrates that pandemic-resistant societal organization can delay the spread of a disease (van Bergeijk 2021, Chapter 6).
-
[6]
See for a comparison with the Great Depression of the 1930s Afesorgbor et al. 2022.
-
[7]
Economic science responded quickly to COVID-19, much quicker than during the Spanish Flu (Boianovsky and Erreygers. 2021). While this is encouraging it is, however, also important to take time as our statistical apparatus, especially the National Accounts, requires processing time. Indeed, revisions of early ‘flash’ estimates of economic activity will bring better coverage and understanding of the sectors and activities that expanded during lockdowns. On top of this standard seasonal adjustment breaks down during a pandemic (Abeln and Jacobs 2021).
-
[8]
The basic reproduction number a.k.a. R0 or ‘R naught’ is the number of new infections that an infected person will generate: new cases per case.
Bibliography
- Abeln, Barend, and Jan P.A.M. Jacobs, 2021, "COVID-19 and Seasonal Adjustment." Cahier Scientific 2021S-05, CIRANO: Quebec.
- Adda, Jerome, 2016, ‘Economic activity and the spread of viral diseases: evidence from high frequency data’, Quarterly Journal of Economics 131 (2), pp. 891–941.
- Afesorgbor, Sylvanus Kwaku, Peter A.G. van Bergeijk and Binyam Afewerk Demena, COVID-19 and the Threat to Globalization: An optimistic note in: in: Elissaios Papyrakis (ed.) Covid-19 and International Development, Springer 2022, in print.
- Agarwal, Ruchir and Gita Gopinath, 2021, A Proposal to End the COVID-19 Pandemic, IMF Staff Discussion Note SDN/2021/004, IMF: Washington DC.
- Akbarpour, Mohammad, Eric B. Budish, Piotr Dworczak and Scott Duke Kominers, 2021, "An Economic Framework for Vaccine Prioritization." paper presented at ICEA After the pandemic – Public policy lessons conference https://iceanet.org/wp-content/uploads/2021/11/Dworczak.pdf
- Allen, Douglas W., 2021, "Covid Lockdown Cost/Benefits: A Critical Assessment of the Literature.", International Journal of the Economics of Business doi :10.1080/13571516.2021.1976051
- Alm, James et al. 2021, ‘Tax Policy Measures to Combat the SARS-CoV-2 Pandemic and Considerations to Improve Tax Compliance: A Behavioral Perspective’ FinanzArchiv/Public Finance Analysis 76 (4), 396-428.
- Baldwin, Richard and Beatrice Weber di Mauro (eds), 2020a Economics in the Time of COVID-19, https://voxeu.org/content/economics-time-covid-19
- Baldwin, Richard and Beatrice Weber di Mauro (eds) 2020b Mitigating the COVID Economic Crisis: Act Fast and Do Whatever It Takes, https://voxeu.org/content/mitigating-covid-economic-crisis-act-fast-and-do-whatever-it-takes.
- Bénassy, Jean-Pascal, 2016,. "Non clearing markets in general equilibrium.", in Matias Vernengo, Esteban Perez Caldentey and Barkley J. Rosser Jr (eds), The New Palgrave Dictionary of Economics (living edition) 10.1057/978-1-349-95121-5_2271-1
- Bergeijk, Peter A.G. van, 2012, Opârg fitfara eft ksvurf, Ekonomiy ur Ďônopros, 72 (8), p. 6.
- Bergeijk, Peter A.G., 2014, Earth economics: An introduction to demand management, long-run growth and global economic governance. Edward Elgar: Cheltenham.
- Bergeijk, Peter A.G. van, 2021, Pandemic Economics, Edward Elgar: Cheltenham.
- Bergeijk, Peter A.G. van and Rolph van der Hoeven (eds), 2017, Sustainable Development Goals and Income Inequality, Edward Elgar: Cheltenham.
- Behsudi, Adam, 2020, ‘Wish You Were Here’, Finance and Development, pp. 36-9
- Boianovsky, Mauro and Erreygers, Guido, 2021, How Economists Ignored the Spanish Flu Pandemic in 1918–20 (February 11, 2021). Center for the History of Political Economy at Duke University Working Paper Series, https://ssrn.com/abstract=3783854 or http://dx.doi.org/10.2139/ssrn.3783854
- Boettke, Peter, and Benjamin Powell, 2021, "The political economy of the COVID‐19 pandemic." Southern Economic Journal 87 (4) blz. 1090-1106.
- Bolt, Jutta and Jan Luiten van Zanden, 2020, ‘Maddison style estimates of the evolution of the world economy. A new 2020 update’, Maddison Project Database, version 2020, Groningen.
- Commission on a Global Health Risk Framework for the Future, 2016, The Neglected Dimension of Global Security: A Framework to Counter Infectious Disease Crises, doi: 10.17226/21891.
- Committee for Development Policy, 2020, Development Policy and Multilateralism after COVID-19, United Nations, New York.
- Cunha, Burk A., 2004, ‘Influenza: historical aspects of epidemics and pandemics’, Infectious Disease Clinics 18 (1), pp. 141–55.
- Dasaratha, Krishna, 2021, Virus Dynamics with Behavioral Responses, paper presented at ICEA After the pandemic – Public policy lessons conference. https://iceanet.org/wp-content/uploads/2021/11/Dasaratha.pdf
- Daszak, Peter, 2012, ‘Anatomy of a pandemic’, The Lancet 380 (9857), pp. 1883–84.
- Davis, C. M., and Wojciech Charemza 2012, Models of disequilibrium and shortage in centrally planned economies. Springer Science & Business Media: New York
- Ebregt, Jos, 2016, "The CPB World Trade Monitor: Technical Description." CPB Background Document, CPB Netherlands Bureau for Economic Policy Analysis: The Hague.
- Fan, Victoria Y., Dean T. Jamison, and Lawrence H. Summers, 2018, ‘Pandemic risk: how large are the expected losses?’, Bulletin of the World Health Organization 96 (2), pp. 129–34.
- Farzanegan, Mohammad Reza, 2021, The Effect of Public Corruption on COVID-19 Fatality Rate: A Cross-Country Examination, CESifo Working Paper No. 8938, Available at SSRN: https://ssrn.com/abstract=3805464
- Gans, J.S., 2021, Vaccine Hesitancy, Passports and the Demand for Vaccination, paper presented at ICEA After the pandemic – Public policy lessons conference. https://iceanet.org/wp-content/uploads/2021/11/Gans.pdf
- Gopinath, G., 2020, ‘Foreword’, in: IMF World Economic Outlook, April 2020, IMF: Washington DC, pp. v–vi.
- Hale, Thomas, et al. 2021, "A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker)." Nature Human Behaviour 5.4 (2021): 529-538.
- Hoeven, Rolph van der and Rob Vos, 2022, Reforming the International Financial and Fiscal System for better COVID-19 and Post-Pandemic Crisis Responsiveness, in: Elissaios Papyrakis (ed.) Covid-19 and International Development, Springer 2022, in print.
- IMF 2018, World Economic Outlook: Challenges to Steady Growth, IMF: Washington DC.
- IMF, 2021, Fiscal Monitor, October 2021: Strengthening the Credibility of Public Finances, IMF: Washington DC.
- Inglesby, Thoma V. et al., 2006, "Disease mitigation measures in the control of pandemic influenza." Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science 4, no. 4 (2006): 366-375.
- International Working Group on Financing Preparedness, 2017, From Panic and Neglect to Investing in Health Security: Financing Pandemic Preparedness at a National Level, https://documents.worldbank.org/en/publication/documents-reports/documentdetail/979591495652724770/from-panic-and-neglect-to-investing-in-health-security-financing-pandemic-preparedness-at-a-national-level
- Jamison, Dean et al. (2018) Disease Control Priorities: Improving Health and Reducing Poverty, World Bank: Washington DC.
- König, Michael and Adalbert Winkler, 2021, ‘The impact of government responses to the COVID-19 pandemic on GDP growth’, PLoS ONE 16(11): e0259362. doi. 10.1371/journal.pone.0259362
- Madhav, Nita, et al., 2017, ‘Pandemics: risks, impacts, and mitigation’, in: Disease Control Priorities: Improving Health and Reducing Poverty, 3rd edition, The International Bank for Reconstruction and Development/The World Bank: Washington DC, pp. 315–45.
- Marugg, Fintan and Tanja Schweinberger, 2021, The impact of social trust on Covid-19 measures in Europe, paper presented at the COVID-19 PHSMs Research Outcome Conference (October 2, 2021).
- Miller, Gay Y., and Katie Parent. "The economic impact of high consequence zoonotic pathogens: why preparing for these is a wicked problem." Journal of Reviews on Global Economics 1 (2012): 47-61.
- Morens, David M. and Anthony S. Fauci, 2007, ‘The 1918 influenza pandemic: insights for the 21st century’, The Journal of Infectious Diseases 195 (7), pp. 1018–28.
- Norman, Joseph, Yaneer Bar-Yam, and Nassim Nicholas Taleb, 2020, ‘Systemic risk of pandemic via novel pathogens–Coronavirus: A note’, New England Complex Systems Institute (2020). https://jwnorman.com/wp-content/uploads/2020/03/Systemic_Risk_of_Pandemic_via_Novel_Path.pdf.
- Politifact, 2020, ‘Are states in a bidding war over medical gear with the feds?’ https://www.politifact.com/article/2020/apr/01/are-states-bidding-war-over-medical-gear-feds/.
- Rasul, Imran, 2020, ‘The economics of viral outbreaks’, American Economic Review AEA Papers and Proceedings 110, pp. 265–8.
- Ritchie, Hanna et al., 2022, - "Coronavirus Pandemic (COVID-19)". Published online at OurWorldInData.org. Retrieved from: 'https://ourworldindata.org/coronavirus' [Online Resource]
- Rowthorn, Robert, and Jan Maciejowski., 2020, "A cost–benefit analysis of the COVID-19 disease." Oxford Review of Economic Policy 36 Supplement 1 (2020): S38-S55.
- Salami, Kolawole, et al, 2020, ‘Meeting report: WHO consultation on accelerating Lassa fever vaccine development in endemic countries, Dakar, 10–11 September 2019’, Vaccine 38 (26), pp. 4135-4141.
- Saltman, Richard B, 2008, "Decentralization, re-centralization and future European health policy." European Journal of Public Health 18 (2), pp. 104-106.
- Sands, Peter, Anas El Turabi, Philip A. Saynisch, and Victor J. Dzau, 2016, ‘Assessment of economic vulnerability to infectious disease crises’ The Lancet 388, no. 10058, pp. 2443-2448.
- Sathyamala, Christina, 2020, COVID-19: a biopolitical odyssey. ISS Working Paper No. 667, Erasmus University ISS: The Hague.
- Seyd, Ben and Bu Feifei, 2021, Perceived Risk Crowds out Trust? Trust and Public Compliance with Coronavirus Restrictions over the Course of the Pandemic, paper presented at the COVID-19 PHSMs Research Outcome Conference (October 2, 2021).
- Shami, Labib and Teddy Lazebnik, 2021, Financing and Managing Epidemiological-Economic Crisis: The Reserve Model, paper presented at ICEA After the pandemic – Public policy lessons conference. https://iceanet.org/wp-content/uploads/2021/11/Shami.pdf
- Smith, Dominic, 2017, ‘Pandemic risk modelling’, The Palgrave Handbook of Unconventional Risk Transfer, Palgrave Macmillan: Cham, pp. 463–95.
- Stoffer, Friso and Peter A.G. van Bergeijk, 2021, Krimp tijdens de COVID-19 pandemie lijkt mee te vallen (Contraction during the COVID-19 pandemic seems to be not too bad; in Dutch), esb.nu. https://esb.nu/blog/20062797/krimp-tijdens-de-covid-19-pandemie-lijkt-mee-te-vallen
- Turner, David, Balázs Égert, Yvan Guillemette, and Jarmila Botev, 2021, "The tortoise and the hare: The race between vaccine rollout and new COVID variants." OECD Economics Department Working Papers, No. 1672, OECD Publishing, Paris
- World Bank, 2014, The Economic Impact of the 2014 Ebola Epidemic: Short- and Medium-Term Estimates for West Africa, World Bank Group, 2014.
- UNCTAD, 2014, World investment report, UN: New York.
- UNCTAD, 2021, Global Investment Trend Monitor, No. 39, https://unctad.org/system/files/official-document/diaeiainf2021d2_en.pdf
- World Bank, 2021, COVID-19 Crisis Through a Migration Lens, Migration and Development Brief 35, https://www.knomad.org/sites/default/files/2021-11/Migration_Brief%2035_1.pdf
- World Health Organization, 2019, Pandemic Influenza Preparedness in WHO Member States: Report of a Member States Survey, World Health Organization: Geneva.
- Wyplosz, Charles, 2020, ‘The good thing about coronavirus’, in: Richard Baldwin and Beatrice Weder di Mauro (eds), 2020a, pp.113–5.
List of figures
Figure 1
Number of pandemics per decade
Figure 2
Covid deaths and median age
Figure 3
Hypothetical death rate of Spanish Flu and COVID-19
Figure 4
Cumulative stringency and COVID-deaths per million population* (G20 countries and world average indicated)
Note * In order to improve readability the figure excludes Peru, Bulgaria, Bosnia and Herzegovina, Hungary, Czechia and Georgia which all had a death rate exceeding 3000 per million inhabitants
Diagram 1
The pandemic trilemma
Figure 5
Number of years where per capita GDP decreased more during 1901-2019 than in 2020
Figure 6
World trade and world industrial production during the Great Recession and the COVID-19 collapse (index numbers; start of crisis=100)
Figure 6a
World merchandise trade
Figure 6b
World industrial production
Figure 7
Gross government debt in percent of regional GDP (1950–2021)
Figure 8
Reduction of reproduction number R and GDP growth due to NPIs in the OECD