Abstracts
Abstract
Fetal Alcohol Spectrum Disorders (FASD) are caused by consumption of alcohol during pregnancy and the prevalence of these disorders in Canada is not well established. Statistics Canada’s Aboriginal Children’s Survey (2006) was used in the current study to assess the prevalence of FASD among Aboriginal children living off reserve across Canada. Characteristics of Aboriginal children with or without a diagnosis of FASD and living in Western Canada were also assessed. Rates of FASD were higher in Alberta and Manitoba than other provinces and territories. For these children who were diagnosed with FASD half received treatment for FASD and treatment rates did not vary across provinces. In Western Canada, FASD was more common among children identified as First Nations, and among older children. Rates of FASD were also higher for Aboriginal children who lived in low income situations, who had experienced food insecurity, or who lived with foster parents. Therefore, Aboriginal children with FASD likely experience other life challenges and these factors should be considered when treating these young children.
Article body
Introduction
Fetal Alcohol Spectrum Disorders (FASD) are a group of serious and preventable conditions caused by maternal consumption of alcohol during pregnancy (Chudley et al., 2005; Elliot, Payne, & Bower, 2006). The consequences of alcohol consumption during pregnancy are a complex interplay between maternal physiology, nutritional status, alcohol dose and timing, and fetal susceptibility. The consequences of prenatal alcohol exposure include Fetal Alcohol Syndrome, Partial Fetal Alcohol Syndrome, Alcohol-Related Neurodevelopmental Disorder, and Alcohol-Related Birth Defect. Understanding more about FASD in Canada is important for both prevention and treatment efforts.
Alcohol use in adulthood has been associated with adverse events in childhood such as abuse (emotional, physical, or sexual), domestic abuse of the mother of the child, parental substance use, mental illness in the home, separation or divorce of parents, and incarceration of a family member (Dube, Anda, Felitti, Edwards, & Croft, 2002). There is a cumulative effect such that the more adverse events or risk factors the more likely a mother is to use substances (Dube et al.; Nair, Schuler, Black, Kettinger, & Harrington, 2003). Aboriginal mothers have been shown to have a high risk of adverse life events that could be associated with substance use during pregnancy. For example, Aboriginal women are more likely than non-Aboriginal women to experience male partner violence (Brownridge, 2003), to be single parents, and to have larger families compared to non-Aboriginal women (Statistics Canada, 2012).
The prevalence of FASD has been estimated at 0.5 to 2.0 per 1000 live births (May & Gossage, 2001). Based on a synthesis of Canadian data, FASD has been shown to be higher in Aboriginal than non-Aboriginal populations in Canada (Tough & Jack, 2011). In studies of sub populations, including children in custody of children’s service, those who encounter the justice system, and among Aboriginal children, rates of FASD ranging from 0.0087% to 23.3% have been found (Tough & Jack). These research findings are mostly from small communities though, and may not be representative of the general population in Canada (Chudley et al., 2005; May et al., 2008). More accurate and more representative prevalence data would assist in determining the influence of interventions designed to reduce FASD and for the design of prevention programs.
Fetal alcohol spectrum disorders require a multidisciplinary team of professionals for an accurate diagnosis (Chudley et al., 2005; Rasmussen, Horne, & Witol, 2006). Early diagnosis of FASD, especially in the preschool years, would provide the opportunity for early intervention (Streissguth, Barr, Kogan, & Bookstein, 1997) so that appropriate treatment can be implemented. Early diagnosis and treatment of FASD is important because children with a FASD diagnosis also typically experience mental health conditions such as attention deficit and hyperactivity disorder (Chudley et al.), cognitive challenges such as low intelligence (Burd, Klug, Martsolf & Kerbeshian, 2003; Premji et al., 2004; Rassmussen et al.; Streisguth et al., 1994), and other secondary disabilities such as educational problems (Robinson, Conry, & Conry, 1987) and trouble with the law (Fast, Conry, & Loock, 1999; Popova, Lange, Bekmuradov, Mihic, & Rehm, 2011). Even though early treatment is important, low and variable service use has been observed among young children living with FASD (Mills, McLennan, & Caza, 2006).
Children with FASD often experience additional threats to their development as a consequence of low socioeconomic status (Bingol et al., 1987) and inconsistent parenting resulting from multiple foster care placements (Fuchs, Burnside, Marchenski, & Mudry, 2007). This suggests that children with FASD likely face additional life challenges throughout development and this may be particularly true for Aboriginal children.
The purpose of the current report was to provide insight into the prevalence and treatment of FASD among Aboriginal children under six years of age in Canada using the 2006 Aboriginal Children’s Survey (ACS) conducted by Statistics Canada. The characteristics of children with FASD in Western Canada and the Territories were also assessed.
Method
The ACS is a post-censal survey of young Aboriginal children (aged 0 to 5) living off reserve in Canada in 2006. For more details on the ACS, consult Statistics Canada’s concepts and methods guide (Statistics Canada, 2008). In 2006, there were approximately 135,000 Aboriginal children in Canada and 76,700 Aboriginal children in Western Canada and the Territories. A sample of these children’s caregivers participated in the ACS and their responses were weighted to infer the entire population of young Aboriginal children living off reserve. While the research and analysis are based on data from Statistics Canada, the opinions expressed do not represent the views of Statistics Canada.
Two analyses were conducted using the ACS. First, FASD diagnosis and treatment prevalence as reported by parents was assessed for provinces when the sample size and estimate was large enough for ethical release from Statistics Canada. The goal of the second analysis was to determine characteristics of Aboriginal children living in Alberta but because the sample size was too small to assess Alberta alone, data from four western provinces (British Columbia, Alberta, Saskatchewan, and Manitoba) and the territories (Yukon, North West Territories, and Nunavut) was combined. This combination enhanced the stability of the estimates and enabled more detailed analysis, as the sample size is larger. The relevance to Alberta was preserved because many of the diagnostic approaches are similar across these jurisdictions (Clarren & Lutke, 2008). Cross tabulations of FASD were generated across age, gender, Aboriginal identity, urban/rural region, low income, food insecurity, and living arrangement.
The child’s Aboriginal identity was reported by a parent or guardian. Aboriginal identity was grouped into three categories: First Nations, Métis, and Aboriginal ancestry. Children who were reported as having an Aboriginal ancestry but were not identified as First Nations or Métis were put into the “Aboriginal ancestry” group. A small proportion of children were identified as both First Nations and Métis; these children were counted in both categories. Low income was defined as families who spend 70% or greater of their before-tax income on basic household necessities (food, shelter, clothing) using the 2006 Census, and known as the Low Income Cut Off in Canada. The food insecurity measure was based on the child having ever experienced hunger due to lack of food. The living arrangement measure was categorized as children living with two parents (including at least one biological), a single parent, with two foster parents, or in alternative living arrangements with relatives or other guardians (Statistics Canada, 2008).
Analyses were conducted at a Statistics Canada Research Data Centre. SAS version 9.2 was used in combination with SAS-callable SUDAAN, version 10.0 for all statistical analyses. Estimations were computed using weighted estimates and variance was computed using ACS survey bootstrapping (1000 weights). Wald F χ2 was used because cross tabulations were categorical and pair wise comparisons were assessed using 95% confidence intervals. The following standard Statistics Canada symbols were used to indicate caution with estimates:
E: The estimate must be used carefully as it is associated with a high level of error.
F: The estimate does not meet Statistics Canada’s quality standards.
Results
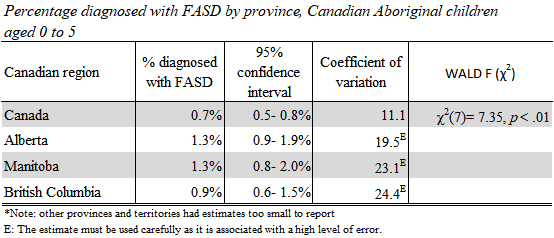
Aboriginal children living in the Western provinces were significantly more likely to have had a diagnosis of FASD with rates in Alberta and Manitoba at 1.3%E, compared to Canadian rates at 0.7% (Table 1). In British Columbia rates at 0.9%E were not significantly different from the other Western provinces or Canadian rates. The other Canadian provinces and territories had FASD rates too small to be reliably reported from the ACS.
Table 1
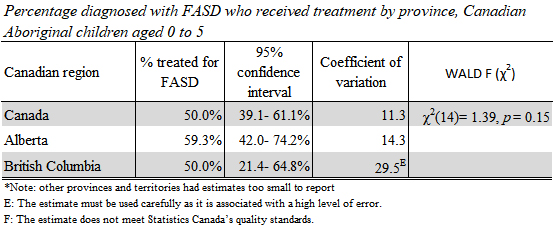
Half of Aboriginal children living in Canada that had received a diagnosis of FASD had received treatment for FASD (50.0%). There was no difference in treatment rates between Alberta (59.3%) and British Columbia (50.0%; Table 2). Too few Aboriginal children were reported to have been diagnosed with FASD in the other provinces and territories to be able to compare treatment rates from these regions.
Table 2
The following analyses are based on Aboriginal children living in Western Canada and the Territories.
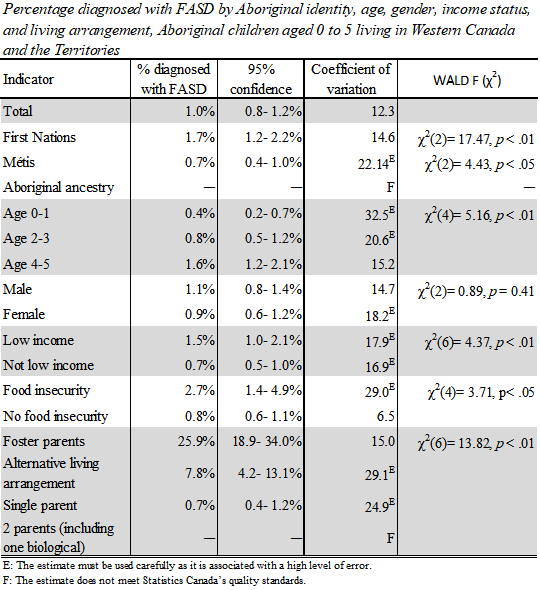
The reported prevalence of FASD among children living in Western Canada and the Territories with a First Nations identity was 1.7% compared to 0.7%E among Métis children; there were not enough children with Aboriginal ancestry (but no Aboriginal identity) diagnosed with FASD to enable reporting within Western Canada and the Territories (Table 3). Children aged four to five years were more likely to be diagnosed with FASD than children under age two (1.6% versus 0.4%E). There were no significant differences in diagnosed FASD by gender (Table 3).
The reported prevalence of FASD among Aboriginal children living in a low income situation was 1.5% compared to 0.7% of children not living in a low income situation (Table 3). Aboriginal children in Western Canada and the Territories who were reported to have experience food insecurity were more than twice as likely to have a diagnosis of FASD (2.7%) compared to Aboriginal children who had never experienced food insecurity (0.8%; Table 3). One in four Aboriginal children living with two foster parents (25.9%) was reported to have been diagnosed with FASD (Table 3). This was substantially higher than the proportion of Aboriginal children in Western Canada and the Territories diagnosed with FASD who were living in alternative arrangements with relatives or non-relatives (7.8%) or living with a single parent (0.7%E; Table 3). The number of Aboriginal children diagnosed with FASD and living with two biological or adoptive parents was too small to report.
Table 3
Discussion
The rates of diagnosis for FASD for Aboriginal children were higher for children living in Alberta and Manitoba compared to the rest of Canada. This finding could be a consequence of true rates of variability across Canada; however, over the last 10 years Alberta, Manitoba, British Columbia, and the Yukon have made significant investments in the development of diagnostic and assessment programs (Clarren & Lutke, 2008), which can lead to identification of more cases.
Approximately half of children diagnosed with FASD were reported to have received treatment for FASD. The low intervention rate for children with FASD is a key finding given the value of early treatment for children diagnosed with FASD for both optimizing current developmental function and for prevention of secondary disabilities (Chudley et al., 2005; Mills et al., 2006; Streissguth, et al., 1997).
In Western Canada and the Territories, older children were found to be more likely to have a diagnosis of FASD most likely because older children had more opportunities to be diagnosed. First Nations children had a higher rate of FASD than children identified as Métis. High rates of FASD have also been found on reserves in Canada in past studies (Robinson, et al., 1987; Square, 1997) however more recent prevalence rates are not available. The rates found among young Aboriginal children living off reserve in the current study were substantially lower than previous on reserve rates from those select communities (1.7% versus 10-19%; Robinson et al.; Square, 1997). Therefore, First Nations children living off reserve had higher rates of FASD (1.7%) than other Aboriginal children in this study (0.7%) but appear to have lower rates than past reports of First Nations children living on select reserves (10-19%).
Many Aboriginal people have elevated exposure to adverse life events such as domestic abuse (Brownridge, 2003), sexual abuse, economic instability (Statistics Canada, 2012), colonization and separation from family (residential school; Stout & Peters, 2011) and these kinds of adverse life events are associated with increased risk of substance abuse (Dube et al., 2002; Hillis et al., 2004). As a consequence of these exposures, First Nations mothers may be at higher risk of entering pregnancy with a substance abuse problem.
Children experiencing economic challenges such as living in low-income situations or experiencing food insecurity were also more likely to be diagnosed with FASD. This indicates that part of the support needed by children with FASD may include addressing basic needs such as access to food. In addition, the risk of alcohol-exposed pregnancies may be addressed in part by early identification of families at risk for adverse events (Tough, 2010) such as economic instability, past history of addiction or past interaction with child welfare. Aboriginal women may be particularly at risk for economic instability due to high rates of lone parent families and large family size (Statistics Canada, 2012).
One in four young Aboriginal children living with foster parents had received a diagnosis of FASD. Fuchs, Burnside, Marchenski, and Mundry (2005) found a similar proportion (17%) of children in Manitoba who were removed from their homes had been diagnosed with (or suspected of) FASD and the majority of children with FASD were Aboriginal. Researchers have previously found that addiction and severity of alcohol use is related to children being placed in foster care, and loss of guardianship is associated with a number of maternal experiences including: psychological distress, history of abuse, less prenatal care (Mills, et al., 2009) as well as economic instability and impaired judgment/emotional stability (Grella, Hser, & Huang, 2006). Indeed, in a recent study by Douzgou and colleagues (2012) 74% of children who were seen for an assessment of FASD were either in care, or cared for by adoptive parents. Additional resources or services for FASD related challenges for foster parents may also be warranted to optimize outcomes for children with FASD.
Rates of FASD according to the national survey are in alignment with work reported by others; however, rates vary across regions in Canada. First Nations children were more likely than Métis children to have been diagnosed with FASD. Furthermore, rates of diagnosis were slightly higher among children living in low income situations or experiencing food insecurity, and much higher among children requiring foster care services indicating that foster parents of children with FASD may benefit from additional support, services, education or training. The reason for the variability in rates should be further evaluated to determine if differences reflect access to diagnostic services, mechanisms for referral, or true differences in the population.
Limitations
The present study was limited in that a non-Aboriginal comparison group was not available for contextual comparisons; the rate of FASD in the young non-Aboriginal population is not known. Diagnoses of FASD were reported by the children’s caregivers and may have been over or under reported. In addition, the diagnostic criteria for FASD requires a multidisciplinary team and consequently, there may be under diagnosis (Nevin, Christopher, Nulman, Koren, & Einarson, 2002; Sokol, Delaney-Black, & Nordstron, 2003).
Appendices
Acknowledgements
Assistance with data analysis by Irene Wong at Statistics Canada’s Research Data Centre was greatly appreciated. We acknowledge that Alberta Human Services (formerly Alberta Children and Youth Services) and the Office of Statistics and Information (OSI) provided access to the Research Data Centre (University of Alberta) to analyze the data from the ACS.
Bibliography
- Bingol, N., Schuster, C., Fuchs, M., Iosub, S., Turner, G., Stone, R.K., et al. (1987). The influence of socioeconomic factors on the occurrence of fetal alcohol syndrome. Advances in Alcohol and Substance Abuse, 6(4), 104-118.
- Brownridge, D.A. (2003). Male partner violence against Aboriginal women in Canada. Journal of Interpersonal Violence, 18(1), 65-83.
- Burd, L., Klug, M.G., Martsolf, J.T., & Kerbeshian, J. (2003). Fetal alcohol syndrome: Neuropsychiatric phenomics. Neurotoxicology and Teratology, 25, 697-705.
- Chudley, A.E., Conry, J., Cook, J.L., Loock, C., Rosales, T., & LeBlanc, N. (2005). Fetal alcohol spectrum disorder: Canadian guidelines for diagnosis. Canadian Medical Association Journal, 172(5 suppl), S1-S21.
- Clarren, S.K., & Lutke, J. (2008). Building clinical capacity for fetal alcohol spectrum disorder diagnoses in western and northern Canada. Canadian Journal of Clinical Pharmacology, 15(2), e223-e237.
- Douzgou, S., Breen, C., Crow, Y.J., Chandler, K., Metcalfe, K., Bronwyn Kerr, J., et al. (2012). Diagnosing fetal alcohol syndrome: New insights from newer genetic technologies. Archives of Disease in Childhood, 97, 812-817.
- Dube, S.R., Anda, R.F., Felitti, V.J., Edwards, V.J., & Croft, J.B. (2002). Adverse childhood experiences and personal alcohol abuse as an adult. Addictive behaviors, 27, 713-725.
- Elliott, E.J., Payne, J., & Bower, C. (2006). Diagnosis of foetal alcohol syndrome and alcohol use in pregnancy: A survey of paediatricians’ knowledge, attitudes and practice. Journal of Paediatrics and Child Health, 42, 698-703.
- Fast, D.K., Conry, J., Loock, C.A. (1999). Identifying fetal alcohol syndrome among youth in the criminal justice system. Developmental and Behavioral Pediatrics, 20(5), 370-372.
- Fuchs, D., Burnside, L., Marchenski, S., & Murdry, A. (2005). Children with disabilities receiving services from child welfare agencies in Manitoba. Retrieved March 12, 2013 from http://cwrp.ca/publications/428
- Fuchs, D., Burnside, L., Marchenski, S., & Murdry, A. (2007). Children with FASD involved with the Manitoba child welfare system. Retrieved March 12, 2013 from http://cwrp.ca/node/591
- Grella, C.E., Hser, Y-I., & Huang, Y-C. (2006). Mothers in substance abuse treatment: Differences in characteristics based on involvement with child welfare services. Child Abuse & Neglect, 30, 55-73.
- Hillis, S.D., Anda, R.F., Dube, S.R., Felitti, V.J., Marchbanks, P.A., & Marks, J.S. (2004). The association between adverse childhood experiences and asolescent pregnancy, long-term psychological consequences, and fetal death. Pediatrics, 113(2), 320-327.
- May, P.A., & Gossage, J.P. (2001). Estimating the prevalence of fetal alcohol syndrome: A summary. Alcohol Research & Health, 25(3), 159-167.
- May, P.A., Gossage, P., Marais, A.-S., Hendricks, L.S., Snell, C.L., Tabachnick, et al. (2008). Maternal risk factors for fetal alcohol syndrome and partial fetal alcohol syndrome in south Africa: A third study. Alcoholism: Clinical and Experimental Research, 32(5), 738-753.
- Mills, R., MT., McLennan, J.D., & Caza, M.M. (2006). Mental health and other service use by young children with fetal alcohol spectrum disorder. Journal of Fetal Alcohol Syndrome International, 4(e1), 1-11.
- Mills, R., MT., Siever, J.E., Hicks, M., Badry, D., Tough, S.C., & Benzies, K. (2009). Child guardianship in a Canadian home visitation program for women who use substances in the perinatal period. Canadian Journal of Clinical Pharmacology, 16(1), e126-e139.
- Nair, P., Schuler, M.E., Black, M.M., Kettinger, L., & Harrington, D. (2003). Cumulative environmental risk in substance abusing women: Early intervention, parenting stress, child abuse potential and child development. Child Abuse & Neglect, 27, 997-1017.
- Nevin, A.C., Christopher, P., Nulman, I., Koren, G., & Einarson, A. (2002). A survey of physicians knowledge regarding awareness of maternal alcohol use and the diagnosis of FAS. BMC Family Practice, 3, 2-5.
- Popova, S., Lange, S., Bekmuradov, D., Mihic, A., & Rehm, J. (2011). Fetal alcohol spectrum disorder prevalence estimates in correctional systems: A systematic literature review. Canadian Public Health Association, 102(5), 336-340.
- Premji, S., Serrett, K., Benzies, K., Hayden, K.A., Dmytryshyn, A., & Williams, A. (2004). The state of the evidence review:Interventions for children and youth with a fetal alcohol spectrum disorder (FASD). Alberta Centre for Child, Family & Community Research. Retrieved March 12, 2013 from http://www.research4children.com/admin/docx/launch.cfm?ItemId=577
- Rasmussen, C., Horne, K., & Witol, A. (2006). Neurobehavioral functioning in children with fetal alcohol spectrum disorder. Child Neuropsychology, 12, 453-468.
- Robinson, G.C., Conry, J.L., & Conry, R.F. (1987). Clinical profile and prevalence of fetal alcohol syndrome in an isolated community in British Columbia. Canadian Medical Association Journal, 137, 203-207.
- Sokol, R.J., Delaney-Black, V., & Nordstrom, B. (2003). Fetal alcohol spectrum disorder. Journal of the American Medical Association, 290(22), 2996-2999.
- Square, D. (1997). Fetal alcohol syndrome epidemic on Manitoba reserve. Canadian Medical Association Journal, 157, 59-60.
- Statistics Canada (2012). Canada yearbook, 2012: Aboriginal peoples (Cat. no. 11-402-XIE). Ottawa.
- Statistics Canada, Social and Aboriginal Statistics Division. (2008). Aboriginal children’s survey, 2006: Concepts and methods guide (Cat. no. 89-634-X No. 006). Ottawa.
- Streissguth, A., Barr, H., Kogan, J., & Bookstein, F. (1997). Primary and secondary disabilities in fetal alcohol syndrome. In Streissguth, A.P., & Kanter, J. (Eds.), The challenge of fetal alcohol syndrome: Overcoming secondary disabilities (pp. 25-39). Seattle, WA: University of Washington Press.
- Streissguth, A., Sampson, P.D., Carmichael Olson, H., Bookstein, F.L., Barr, H.M. Scott, M., et al. (1994). Maternal drinking during pregnancy: Attention and short-term memory in 14-year old offspring- A longitudinal prospective study. Alcoholism: Clinical and Experimental Research, 18(1), 202-218.
- Stout, R., & Peters, S. (2011). Kiskinohamâtôtâpânâski: Inter-generational effects on professional First Nations women whose mothers are residential school survivors. Prairie Women’s Health Centre of Excellence. Retrieved March 12, 2013 from http://www.trc.ca/websites/trcinstitution/File/pdfs/kiskino_Intergenerational%20Effect%20of%20IRS%20on%20Prof%20Women.pdf
- Tough, S.C. (2010). Dispelling myths and developing a framework for reducing the risk of alcohol-exposed pregnancies. Oxford Forum on Public Policy. Retrieved March 12, 2013 from http://forumonpublicpolicy.com/spring2010.vol2010/spring2010archive/tough.pdf
- Tough, S.C., & Jack, M. (2011). Frequency of FASD in Canada, and what this means for prevention efforts. In Riley, E.P., Clarren, S., Weinberg, J., & Jonsson, E. (Eds.), Fetal alcohol spectrum disorder (pp. 27-43). Weinheim, Germany: Wiley-VCH Verlag & Co.
List of tables
Table 1
Table 2
Table 3